© Center for Endometriosis Care/Ken Sinervo MD, MSc, FRCSC. All rights reserved. No reproduction permitted without written permission. Date of original publication: 1991. Most current revision: 2024. No external funding was utilized in the creation of this material. The Center for Endometriosis Care neither endorses nor has affiliation with any resources cited herein. The following material is for informational purposes only and does not constitute medical advice.
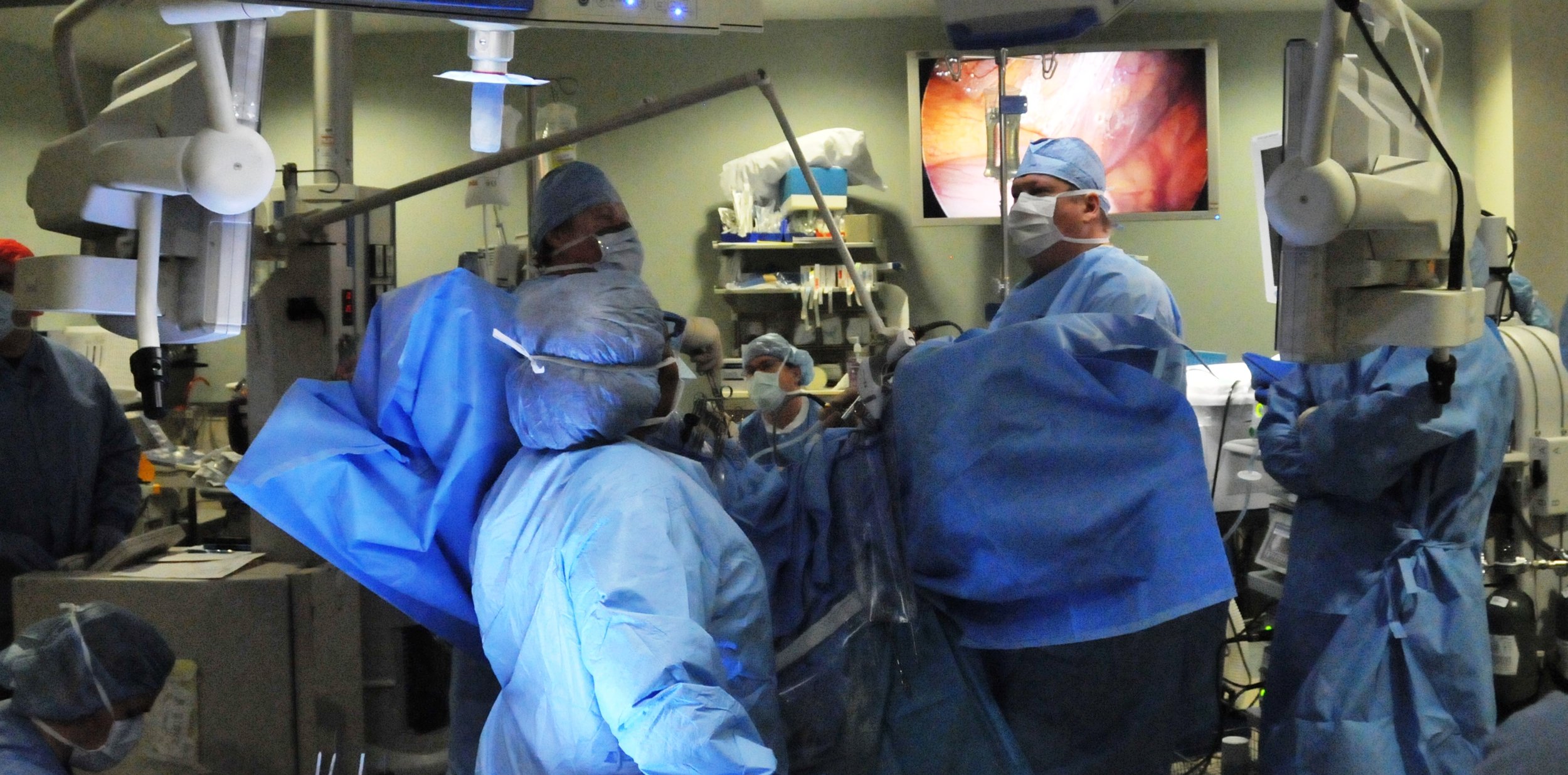
Surgery - and any/all interventions for endometriosis - remains the decision of the patient and there are no universal, guaranteed outcomes. This article discusses the specific modality of Laparoscopic Excision (LAPEX) as the surgical cornerstone of any high quality, integrative approach to treating endometriosis. This does not imply that all endometriosis patients are candidates for, or will benefit from, surgical (or any other) intervention of any kind. Every case should be approached on its own merits in careful consultation with the patient through a robust informed consent process. Read on for common discussion points surrounding this topic and also check out "Dr Albee on Excision and What To Expect For Your Surgery At The CEC by Wendy Winer, RN, BSN, CNOR, RNFA.
What is “Excision Surgery”?
The Oxford Dictionaries define excision as: “to cut out surgically; to remove by cutting. Late 16th century (in the sense 'notch or hollow out'): from Latin excis- 'cut out', from the verb excidere, from ex- 'out of' + caedere 'to cut'.” The CEC was established over three decades ago as one of the first Centers of Expertise anywhere in the world, specializing in and refining the excisional approach to effectively treating the disease. We have treated thousands of patients from nearly 70 countries to date, performing over 13,000 combined procedures, with excellent long-term outcomes among the majority of those in our care.
Generally speaking, LAPEX allows for endometriosis to be cut out from affected areas without damaging surrounding structures or removing otherwise healthy tissue or organs. Again, however: not everyone is a candidate for surgery and excision is not a definitive/universal “cure.” Our experience, however, echoes the scientific literature in that LAPEX has been demonstrated to be associated with improved pain and quality of life for many individuals [Rindos et al., 2020; Pundir et al. 2017; Yeung 2014].
Rindos NB, Fulcher IR, Donnellan NM. Pain and Quality of Life after Laparoscopic Excision of Endometriosis. J Minim Invasive Gynecol. 2020 Nov-Dec;27(7):1610-1617.e1.
Pundir J, Omanwa K, Kovoor E, Pundir V, Lancaster G, Barton-Smith P. Laparoscopic Excision Versus Ablation for Endometriosis-associated Pain: An Updated Systematic Review and Meta-analysis. J Minim Invasive Gynecol. 2017 JulAug;24(5):747-756.
Yeung P Jr . The laparoscopic management of endometriosis in patients with pelvic pain. Obstet Gynecol Clin North Am. 2014 Sep;41(3):371-83.
Is Every Doctor Who Treats Endometriosis an “Endo Specialist?”
No. As defined by Healthcare.gov, a physician specialist is a practitioner who “focuses on a specific area of medicine or a group of patients to diagnose, manage, prevent or treat certain types of symptoms and conditions.” Despite lengthy efforts to formally designate endometriosis as a true medical subspecialty, to date no such institutional accreditation or legitimate ‘vetting’ exists; therefore, anyone may call themselves an ‘endo specialist’ and the term is far too often broadly utilized, especially on social media and by marketing-driven ‘vetting platforms.’ The emphasis, however, should be on those who can actually demonstrate high volume, significant levels of knowledge, skill and dedicated care for the disease; it is in that context we use the term ‘specialist’ throughout this article.
Isn’t Excision Just a Marketing Ploy, Experimental, or New?
No. Termed decades ago by famed endometriosis expert Professor Ray Garry [2004] as “the 'gold standard' approach for the management of endometriosis,” excision is not new, experimental, investigational, or a ‘marketing ploy.’ It is the well-established surgical component of a multidisciplinary approach to treating the disease. Dedicated endometriosis Centers like ours have been using the excisional approach for decades - long before the Internet and social media brought the technique to the forefront of the treatment discussion. The framework behind the principles of Laparoscopic surgery itself was even reported more than a century ago, and throughout the mid 1800's many scientists attempted to construct endoscopic-style instruments. Jumping to the early 1930's, the first reports of Laparoscopic interventions for non-diagnostic purposes were published (initial procedures included lysis of adhesions and biopsies of abdominal organs under direct visualization). Camran Nezhat, MD first reported video Laparoscopic treatment of advanced stage endometriosis in 1985 [Nezhat C., 2010]. After 1986, development of video chips facilitating magnification and projection of the surgical field led Laparoscopic surgery to become the vital part of our surgical discipline it is today. Prof Dr Erich Mühe of Germany performed the first Laparoscopic Cholecystectomy in 1985, followed by Phillipe Mouret in 1987 and Francois Dubois in 1988 [Reynolds, 2001]. From then through now, Laparoscopy has “changed the field of surgery more drastically and more rapidly than any other surgical milestone” [Spaner et al., 1997].
Even as far back as the 1850s, physicians were noted to ‘dig out the endometriosis nodules with blunt scissors or even with their own fingernails’ [Nezhat et al., 2012]. TeLinde & Scott [1952] further defined the surgical objectives of treatment of endometriosis over 70 years ago: “one should EXCISE…all evident endometriosis.” While it is also true that pain can persist and recurrence/persistence of disease can occur after excision, we can expect the latter to be much higher in non-excisional cases.
Endometriosis should also be excised even if hysterectomy is performed, as probability of pain persistence post-hysterectomy ranges around 15% and risk of pain worsening is between 3%-5%, with a six-time higher risk of further surgery in those patients with ovarian preservation as compared to ovarian removal. Hysterectomy may even be unnecessary, despite endometriosis being a leading cause of the 600,000 hysterectomies performed annually in the U.S., as healthy tissue and organs may be spared through the Laparoscopic Excision approach [Berlanda et al., 2010]. Given the technically difficult, highly advanced surgical skills needed, however, excision should be performed only in specialized high-volume centers by high-volume surgeons; such skill and volume become even more critically important when persistent, bowel, bladder and/or extrapelvic disease are involved. Any surgeon of integrity will tell you their goal is to actually limit repeat surgical interventions as much as possible. No responsible, ethical surgeon wants to make a patient undergo unnecessary, invasive surgeries! Surgery, and repeat surgery, are not always appropriate; when they are, on a case-by-case basis, the procedure should be as minimally invasive as possible and done for the right reasons by a skilled surgeon to avoid future reoperation where and whenever possible.
Garry R. The effectiveness of laparoscopic excision of endometriosis. Curr Opin Obstet Gynecol. 2004 Aug;16(4):299-303.
Nezhat C. My journey with the AAGL. J Minim Invasive Gynecol. 2010;17(3):271–277.
Reynolds W Jr. The first laparoscopic cholecystectomy. JSLS. 2001 Jan-Mar;5(1):89-94.
Spaner SJ, Warnock GL. A brief history of endoscopy, laparoscopy, and laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 1997 Dec;7(6):369-73.
Nezhat C, Nezhat F, Nezhat C. FertilSteril Volume 98, Issue 6, Supplement, S1-S62, December 2012.
TeLinde RW, Scott RB. Diagnosis and treatment of endometriosis. G.P. Am Academy of General Practice 1952; 5: 61 – 65.
Berlanda N, Vercellini P, Fedele L. The outcomes of repeat surgery for recurrent symptomatic endometriosis. Curr Opin Obstet Gynecol. 2010;22(4):320-325.
Is Excision Surgery the Cure for Endometriosis?
We do not use the word “cure” in relation to ANY treatments for endometriosis. However, excision is the ‘gold standard’ for surgically treating the disease - especially deep endometriosis [Byrne et al., 2018] - and can be very effective at conferring relief for many who undergo the procedure. However, it is also true that not all pain is from endometriosis; that even removing all disease may not solve underlying issues for some; and that removal of endometriosis alone will not necessarily address other conditions which lend themselves to pain or symptoms. Perhaps more important than use of the word ‘cure' is addressing each patient’s concerns in a patient-centric, collaborative way to provide the best functional outcome for long-term relief and restoration of quality of life in that individual.
Byrne D, Curnow T, Smith P, Cutner A, Saridogan E, Clark TJ; BSGE Endometriosis Centres. Laparoscopic excision of deep rectovaginal endometriosis in BSGE endometriosis centres: a multicentre prospective cohort study. BMJ Open. 2018 Apr 9;8(4):e018924.
Does Excision Universally Prevent Recurrence or Persistence of Endometriosis?
No. Like all surgeons, we have a number of patients - around 10-20% - who return to us for another surgery or have surgery elsewhere with findings of recurrent or persistent endometriosis. We work with our patients to ensure we are addressing the 'big picture' of their individual situation and routinely engage in collaborative referrals ranging from imaging (which we also perform) to physical therapy to pain management to dietary approach and beyond to make sure a true integrative approach is used. We also strive every day to increase disease awareness, provide training and elevate endometriosis to a priority public health platform in order to improve the time to diagnosis and effective, early - and proper - treatment for all those affected. Through timely intervention, individuals can be diagnosed and treated sooner, avoiding the vicious cycle of repeated drug therapies and ineffective surgeries that routinely characterize the disease. By educating society, legislators, insurers and the public, and by training tomorrow's providers, we can empower patients and remove the ubiquitous barriers to care that continue to exist - and one day, perhaps even make endometriosis a preventable disorder. In summary, though universal "cure" for every single individual with the disease may remain elusive, LAPEX remains a critical, effective part of the treatment picture for this disease. Many of our patients routinely report to us that they are painfree, many years after their surgeries.
Can’t Endometriosis be Diagnosed & Treated without Surgery?
A growing trend towards “medical diagnosis” (aka “clinical diagnosis”) driven by various ‘guidelines’ is gaining popularity. However, it is not possible to obtain biopsy-proven confirmation without surgical intervention. Whether, when, and how to proceed is the patient’s choice in the context of their own situation. It is also imperative to understand that pain - pelvic pain in particular - has many generators, and endometriosis often presents with a unique constellation of symptoms and may be accompanied by other conditions; nor should non-classic signs be undervalued, i.e., soft tissue, lung or diaphragmatic disease; bowel or bladder-only symptoms, etc. Dismissing these indications and hindering access to timely confirmative diagnosis and treatment - which can and should be accomplished in the same surgical encounter - only confound the patient’s scenario further. In addition, a ‘non-biopsy approach’ to diagnosis dilutes the research effort; conducting studies on uncertain or induced “endometriosis” leads to uncertain results and hinders progress. It is of course prudent to rule out differential diagnoses and use all tools in the armamentarium, but physical examination, imaging and lab studies related to an endometriosis diagnosis are heavily operator-dependent and commonly have poor sensitivity, specificity and predictive values. Hence, absence of evidence is not evidence of absence. The choice to intervene medically or surgically should be the patient’s after fully informed consent and thorough discussion of the pros and cons of all approaches.
Just as it matters who reads and interprets imaging and other studies, who performs the surgery, how and when is of critical importance, as excision is a highly advanced surgical technique requiring extensive training. Likewise, accuracy in diagnosis and treatment is dependent on the ability of the surgeon to recognize disease in all its different manifestations. This means, if the surgeon is not familiar with all signs of endometriosis including those less common such as subtle areas of peritoneal tension, atypical clear vesicles, extrapelvic endometriosis, etc. then disease will be missed and left behind untreated; surgeons can only see and treat what they recognize. It is also imperative that a patient-centric, judicious - even conservative - approach is utilized; planning each individual’s case based on their very specific needs and desired outcomes is critical. Endometriosis treatment is not one-size-fits-all, and patients need a specialist who will work with them on a personalized care plan - when the plan involves surgery, it is imperative the surgery be performed by those with advanced skill.
My Surgeon Performed Laser Surgery. Is that Excision? What about Robotic Assisted Surgery? Which is Better?
All surgeons - and surgeries - are not equal. Significant confusion often persists around the surgical approaches for endometriosis. The laser is a tool, not a method. Laparoscopy is a surgical approach, not a tool. It is important to understand that tool and method are not nearly as important as skill of the surgeon: if they cannot excise, they cannot excise using any method or tool. Be sure you know which approach they are using. For example, the laser can be used to safely and successfully perform Laparoscopic resection (excision) of all disease, as we have pioneered here in Dr Sinervo’s Center – or it can be used to superficially and incompletely burn or ablate surface lesions and leave disease behind as many obgyn generalists do. The approach and tool are not nearly as important as the skill of the surgeon who uses them.
Laser ablation (not to be confused with uterine ablation, a different procedure entirely) and other superficial methods commonly performed by non-excisionists merely char surface tissue, making microscopic evaluation impossible and often leaving behind endometriosis – which may lead to recurrence and potential complications in future surgical interventions. In one study, for example, improvement in most symptom measures and quality of life indicators was found in endometriosis patients following excision, as compared to the ablation technique in which participants indicated either no improvement or a worsened symptom and quality of life status [Mackenzie, 2023]. Excision is not typically performed for endometriosis treatment outside the tertiary specialty centers, though the technique has been commonly used for a multitude of surgical conditions almost since the inception of surgery itself, so be sure to ask questions. It’s imperative to determine which method your surgeon will be using and understand their disease knowledge, approach and expected outcomes.
Mackenzie M. Laparoscopic Excision Vs Ablation: “Endometriosis Facebook” Symptom And Qol Questionnaire Results. AJOG. Volume 228, Issue 3, Supplement, S901-S902, March 2023.
Why is Endometriosis So Poorly Managed in General?
Stark and persistent misunderstandings and biases continue to surround endometriosis. Often dismissed as simply ‘killer cramps’ that are ‘normal’, or worse - ‘in your head,’ the disease causes considerable negative impact on quality of life, especially in the domains of pain and psychosocial functioning [Culley et al., 2013]. Endometriosis can also cause physical and psychological damage when left untreated or treated unsuccessfully [Dell'oro et al., 2013]…yet an incalculable lack of disease knowledge persists. In the general healthcare community including at the OB/GYN level, for example, it is taught (and hence practiced) that the most frequent mainstays of treatment are medical suppressives and ablative surgery. While always an option for those who desire it, patients should understand that medication does not eradicate endometriosis. The disease does not simply ‘go away’ as a result of drug suppression. At best, such a course of therapy provides only a temporary means of symptom improvement, not definitive treatment. Often, side effects of many endometriosis drug therapies are significantly negative and intolerable, and may last far beyond the cessation of treatment. Poor outcomes on suppression therapies are routine and drug therapy that can destroy endometriosis permanently has yet to be discovered. Hormonal suppression has “no effect on adhesion of endometriotic cells and cannot improve fertility” [Aznaurova et al., 2014], and success of said therapies may be dependent on localization/type of lesions, with superficial peritoneal/ovarian disease responding better than deep/infiltrative disease. Still, despite evidence to the contrary, some providers prefer - and impose their preference on to their patients - the option of medical management and even “diagnosis” by undertaking a strategy of ‘treat without seeing.’
In the majority of such cases, further diagnostic and definitive treatment delays – and patient dissatisfaction – are highly common. The best such medications can do is suppress the disease on a short-term basis, and symptoms undoubtedly recur at cessation of therapy. Suppressive therapies are further limited in usefulness by the length of time they can be safely taken (usually six-twelve months), their high cost, and commonly incapacitating side effects. Hence, the sooner in an individual’s life the disease can be correctly diagnosed and truly eradicated, the better their long-term outlook becomes.
Poor surgical outcomes also remain commonplace. Incomplete or poorly done surgery means the patient must still deal with any residual symptoms of the endometriosis left behind. Many times, "limited surgery" results in skimming/burning the top off the area of deep disease, leaving behind the bulk of endometriosis. This is not excisional and allows for subsequent adhesion formation to bury remaining disease. Disease covered by new adhesions increases pain, leaving a very dissatisfied patient. Burning/ablation, coagulation and other superficial approaches – without or without medical suppression - routinely result in poor outcomes and inevitably require costly reoperation in the future, subjecting the patient to additional procedures, increased expense and surgical risks – yet this sadly remains the ordinary approach to endometriosis. Still, there is hope!
Surgery (when appropriate, in the proper hands, and for the right patient), alternative therapies, diet and nutrition, acupuncture, physical therapy, medications, and other adjuncts can all be helpful for symptom management. As noted, we believe high-quality, minimally invasive excisional surgery is the key to building an effective plan. One need only spend time immersed in the patient population to realize the far-reaching physical and emotional impact of the disease and the toll repeated surgical and medical interventions take, though the literature is often far removed from such first-hand experience(s). Above all, genuine compassion for those who battle this insidious illness must be present.
Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, Raine-Fenning N. The social and psychological impact of endometriosis on women's lives: a critical narrative review. Hum Reprod Update. 2013 Nov-Dec;19(6):625-39.
Dell'oro M, Collinet P, Robin G, Rubod C. Multidisciplinary approach for deep endometriosis: interests and organization. Gynecol Obstet Fertil. 2013 Jan;41(1):58-64.
Aznaurova YB, Zhumataev MB, Roberts TK, Aliper AM, Zhavoronkov AA. Molecular aspects of development and regulation of endometriosis. Reprod Biol Endocrinol. 2014 Jun 13;12:50.
Why Don’t Specialty Excision Centers Accept Insurance for Excision Surgery?
This is a highly misunderstood premise. Many excision centers including ours DO accept insurance, as an out of network provider. We, like other specialists in the disease and various other health subspecialties, are not ‘cash only’ and certainly accept out of network benefits. To better understand insurance and endometriosis care in a specialty center, please read on:
Insurers have requirements for how the doctor practices. They incentivize quantity over quality, encourage policy holders to seek cheaper - yet possibly subpar - care with clinicians who do not specialize in the disease and routinely do not reimburse or reward high quality treatment, with complicated reimbursement strategies (and penalties); all done while cutting the patient out of the process. Surgical destruction of endometriosis by any means shares the same universal billing code (CPT) and henceforth is reimbursed accordingly. That is to say, excision is not - but should be! - categorized as its own CPT, something we have been lobbying for strongly for years; or at the very least, reimbursed accordingly to lesser surgical removal like coagulation, etc. To that end, our current healthcare system rewards an approach of untreated/poorly treated disease – leading to certain failure and need for retreatment, thus incurring additional costs and subjecting the patient to ongoing care. This failed bureaucracy contributes greatly to the ever-growing fiscal burden the disease imposes on society – and the patient.
As we have said for years, reimbursement for endometriosis is a broken system:
No incentives exist to improve quality of - or perform specialized – treatment for endometriosis;
The current system rewards an approach towards untreated/poorly treated disease; and
Surgeons should not be punished or forced to offer subpar care to their patients based on the ill-informed assumptions and decisions made by those who do not understand this disease (e.g., payers).
This protocol is a huge disservice and accounts for lack of reimbursement strategies which would otherwise accurately reflect the true nature of the disease and the critical need for highly skilled surgeons to treat it. Unfortunately, referrals and reimbursements to the specialist centers like ours are often withheld injudiciously due to lack of understanding about the disease and are based loosely on outdated beliefs and unproven concepts, not least of which include the framing of endometriosis as simply normal tissue in abnormal locations and other flawed notions that have largely been based on underpowered studies.
What being ‘out of network’ means in the context of our practice: we work for our patients, not the insurance companies. Although we are a specialized surgical practice that routinely employs ever-improving teamwork, communication and readiness for our cases, we are able to increase productivity and maximize outcomes while actually decreasing costs. Without the red tape of who/when/how long/what for, we can provide personalized, continuous care through both quality outcomes and cost-containment – and by working one on one with our patients to offer individualized, compassionate care based on the specifics of their own case (this includes discounts for many of patients). We also do first check, file all the paperwork, handle the appeals and everything an in-network provider would do. Learn more about insurance and treatment at the CEC here.
How Do I know If Excision is Right for Me?
Again, not everyone is a candidate for surgery of any kind, and there are no guarantees that excision - or any treatment at all - will confer total relief. However, based on our decades-long experience in operating on the countless advanced cases of endometriosis that we treat and managing the complex care of thousands and thousands of our patients from every corner of the world, we expect that the majority of those for whom surgery is indicated will find improvements in quality of life and overall functioning (as well as fertility, if desired). We must first evaluate the patient’s case, however, and review all the factors of their personal situation, which we will gladly do for free through our initial case review. We will provide a thorough evaluation and offer our honest opinion about the likelihood for expected outcomes in our surgical candidates.
I Had Excision Surgery but did not Obtain Relief. What’s Going on??
There is perhaps nothing more frustrating and upsetting than feeling like your ‘best-hope-for-relief-surgery’ didn’t work. This is a multifaceted, complex issue that may occur – even following excision in the hands of a specialist. While this matter has to be discussed with one’s surgeon directly to determine the next best steps for the indivdual, we have an article topically addressing this topic here for preliminary information.
Do you have any References Supporting the use of Excision?
Following is a small sampling from the greater body of scientific literature on excision and surgery for endometriosis dating back 30+ years:
"Endometriosis surgery needs to balance completeness of excision and prevention of complications during and after surgery while preserving bowel and bladder function and fertility. This multifactorial decision needs surgical judgment, based on the knowledge of anatomy and of the disease endometriosis, and varies with the skills and experience of the surgeon." Koninckx PR, Fernandes R, Ussia A, Schindler L, Wattiez A, Al-Suwaidi S, Amro B, Al-Maamari B, Hakim Z, Tahlak M. Pathogenesis Based Diagnosis and Treatment of Endometriosis. Front Endocrinol (Lausanne). 2021 Nov 25;12:745548.
"The surgical excision of endometriosis is indicated after failure of medical treatment and when lesions become symptomatic by impairing bowel, urinary, sexual, and reproductive functioning." Casas SGL, Spagnolo E, Saverio SD, Álvarez-Gallego M, Carrasco AL, López MC, Cobos ST, Campo CF, Gutiérrez AH, Miguelañez IP. Short-term outcomes in patients undergoing laparoscopic surgery for deep infiltrative endometriosis with rectal involvement: a single-center experience of 168 cases. Ann Coloproctol. 2023 Jun;39(3):216-222.
"The treatment of endometriosis requires complete resection of the endometriotic lesion. In the case of ectopic endometriosis, complete excision of the round ligament by laparoscopic surgery may be useful if the lesion extends into the abdominal cavity via the round ligament. In the case of inguinal ectopic endometriosis involving the canal of the Nuck, it is important to completely remove the mass." Mushiake S, Kawaguchi N, Asakuma M, Komeda K, Shimizu T, Hirokawa F, Shimomura T, Lee SW. The usefulness of laparoscopic surgery for inguinal endometriosis. Surg Case Rep. 2023 Jan 26;9(1):12.
"Timely surgical intervention in the form of complete endometriosis excision and decompression of the sciatic nerve can prevent significant neurological damage due to the associated adhesions, fibrosis and the compression caused by endometriotic tissue over the sciatic nerve." Bindra V, Nori M, Reddy R, Reddy R, Satpathy G, Reddy CA. Sciatic nerve endometriosis - The correct approach matters: A case report. Case Rep Womens Health. 2023 May 19;38:e00515.
"Surgical resection of the lesion should be performed in order to remove the lesion and to confirm the diagnosis histologically." Sarpietro G, Matarazzo MG, Vecchio GM, Palermo G, Cianci A. Primary vulvar endometriosis in postmenopausal woman: a case report and review of the literature. Minerva Obstet Gynecol. 2023 Aug;75(4):387-389.
"Up to 28% of patients may require a repeated surgical procedure during the 10 years after complete excision of endometriosis. Conservation of the uterus is followed by an increased risk of repeated surgery." Roman H, Chanavaz-Lacheray I, Hennetier C, Tuech JJ, Dennis T, Verspyck E, Merlot B. Long-term risk of repeated surgeries in women managed for endometriosis: a 1,092 patient-series. Fertil Steril. 2023 Oct;120(4):870-879.
In a study of 207 individuals undergoing Laparoscopic Excision for bladder endometriosis between 1998-2019, authors found that 'removal [excision] was feasible, with very low complications rates and high associated postoperative pregnancy rates.' Soares M, Luyckx M, Maillard C, Laurent P, Gerday A, Jadoul P, Squifflet J. Outcomes after Laparoscopic Excision of Bladder Endometriosis Using a CO2 Laser: A Review of 207 Cases in a Single Center. J Minim Invasive Gynecol. 2023 Jan;30(1):52-60.
“It is important for reducing of long-term complication like rectal endometriosis that complete and safe excision of pelvic endometriosis with expert surgical strategy.” Kwack JY, You SK, Kwon YS. Diagnosis and surgical treatment of isolated rectal endometriosis: long term complication of incomplete treatment for pelvic endometriosis. Pak J Med Sci. 2016 May-Jun;32(3):789-92.
“...Conversely, when bladder nodules are treated by cystoscopy alone, resection may be incomplete. A combined laparoscopic-cystoscopic approach allows safe and controlled resection. The video reports the procedure performed in a 33 year-old primipara who presented with a 40mm bladder nodule. The laparoscopic step is carried out by the gynecologist, who separates the bladder from the uterus and opens the vesico-vaginal space. Concomitantly, the urologist identifies and circumscribes the nodule's limits by cystoscopy. Then, the gynecologist identifies the circular incision previously performed, and completes the resection. The bladder defect is sutured. Early and mid-term postoperative outcomes were uneventful. In patients with large nodules of the bladder, combined laparoscopic-cystoscopic approach allows complete resection of endometriosis lesion, preserves healthy bladder tissue and avoids inadvertent injury of ureters.” Millochau JC, Stochino-Loi E, Defortescu G, Darwish B, Roman H. Combined laparoscopic and cystoscopic approach in large deep infiltrating endometriosis of the bladder. J Gynecol Obstet Hum Reprod. 2017 Nov;46(9):691-692.
“Concerning the surgical approach, it appears that laparoscopy should be the first option; the laparoscopic robot-assisted route can also be proposed. The techniques of rectal shaving, discoid resection and segmental resection are the three techniques used for surgical excision of colorectal endometriosis. The parameters taken into account for the use of either technique are: the surgeon's experience, the depth of infiltration of the lesion within the rectosigmoid wall, the lesion size and circumference, multifocality and the distance of the lesion from the anal margin. In the case of deep endometriosis with colorectal involvement, performing an incomplete surgery increases the rate of pain recurrence and decreases postoperative fertility.” Ballester M, Roman H. Prise en charge chirurgicale de l’endométriose profonde avec atteinte digestive, RPC Endométriose CNGOF-HAS [Surgical management of deep endometriosis with colorectal involvement: CNGOF-HAS Endometriosis Guidelines]. Gynecol Obstet Fertil Senol. 2018 Mar;46(3):290-295.
"5162 women of reproductive age with rectovaginal endometriosis of which 4721 women had planned laparoscopic excision (Laparoscopic surgical excision of rectovaginal endometriosis requiring dissection of the pararectal space)...At 6 months postsurgery, there were significant reductions in premenstrual, menstrual and non-cyclical pelvic pain, deep dyspareunia, dyschezia, low back pain and bladder pain. In addition, there were significant reductions in voiding difficulty, bowel frequency, urgency, incomplete emptying, constipation and passing blood. These reductions were maintained at 2 years, with the exception of voiding difficulty. Global quality of life significantly improved from a median pretreatment score of 55/100 to 80/100 at 6 months. There was a significant improvement in quality of life in all measured domains and in quality-adjusted life years. These improvements were sustained at 2 years. All analgesia use was reduced and, in particular, opiate use fell from 28.1% prior to surgery to 16.1% at 6 months. The overall incidence of complications was 6.8% (321/4721). Gastrointestinal complications (enterotomy, anastomotic leak or fistula) occurred in 52 (1.1%) operations and of the urinary tract (ureteric/bladder injury or leak) in 49 (1.0%) procedures. Laparoscopic surgical excision of rectovaginal endometriosis appears to be effective in treating pelvic pain and bowel symptoms and improving health-related quality of life and has a low rate of major complications when performed in specialist centres." Byrne D, Curnow T, Smith P, Cutner A, Saridogan E, Clark TJ; BSGE Endometriosis Centres. Laparoscopic excision of deep rectovaginal endometriosis in BSGE endometriosis centres: a multicentre prospective cohort study. BMJ Open. 2018 Apr 9;8(4):e018924.
“Although lesions suspicious for endometriosis may have differing rates of positive pathology based on appearance, no lesion characteristic was able to exclude the possibility of endometriosis. In addition, hormone use may influence lesion appearance at the time of surgery, with clear lesions more prevalent. These data have implications for appropriate identification of endometriosis at the time of laparoscopy to ensure accurate diagnosis and complete treatment of disease.” Weng CS, Cope AG, Mara KC, Schoolmeester JK, Khan Z, Burnett TL. Association Between Laparoscopic Appearance of Superficial Endometriosis, Positive Histology, and Systemic Hormone Use. J Minim Invasive Gynecol. 2022 Dec;29(12):1339-1343.
"Endometriosis is a benign, but potentially serious gynaecological condition in terms of abdominal pain and impaired fertility. Laparoscopic excision techniques are considered the therapeutic standard...endometriosis is preferably treated laparoscopically. For the therapy of deep-infiltrating endometriosis, guidelines favour excision over ablative techniques." Keckstein JS, Keckstein S, Brunecker K, Neugebauer A, Nüssle D, Hoffmann S, Andress J, Neis F, Scharpf M, Enderle M, Rothmund R, Brucker SY, Jun MW, Kraemer B. Hybrid argon plasma coagulation (HybridAPC) versus sharp excision for the treatment of endometriosis: a prospective randomized clinical trial. Arch Gynecol Obstet. 2023 Jan;307(1):187-194.
"The study demonstrates that laparoscopic bladder endometriosis removal [laparoscopic resection] is feasible with very low complications rates and was associated with high PR (both spontaneous and in vitro fertilization), even in patients with previous infertility. BE recurrence is lower than for other endometriosis locations." Soares M, Luyckx M, Maillard C, Laurent P, Gerday A, Jadoul P, Squifflet J. Outcomes after Laparoscopic Excision of Bladder Endometriosis Using a CO2 Laser: A Review of 207 Cases in a Single Center. J Minim Invasive Gynecol. 2023 Jan;30(1):52-60.
"Clinicians may misdiagnose inguinal endometriosis as a hernia, lipoma, or hematoma. Preoperative diagnosis relies on a careful medical review and a detailed physical examination. Complete surgical excision is the curative treatment* and prevents recurrence." Mushiake S, Kawaguchi N, Asakuma M, Komeda K, Shimizu T, Hirokawa F, Shimomura T, Lee SW. The usefulness of laparoscopic surgery for inguinal endometriosis. Surg Case Rep. 2023 Jan 26;9(1):12. (*As stated by authors)
"The laparoscopic resection of the ureteral endometriosis could be suggested as a feasible and safe method associated with favorable functional outcomes." Alborzi S, Askary E, Poordast T, Alborzi S, Abadi AKH, Shoaii F. Approach to ureteral endometriosis: A single-center experience and meta-analysis of the literature. J Obstet Gynaecol Res. 2023 Jan;49(1):75-89.
"Surgical resection for negative margins is the main treatment, and permanent impairment of function may occur in a few patients due to delayed diagnosis." Ye H, Shen C, Quan Q, Xi M, Li L. Endometriosis of the skeletal muscular system (ESMS): a systematic review. BMC Womens Health. 2023 Jan 26;23(1):37.
"This case highlights that the gynecologist who performs laparoscopic excision of DIE should be well expertized and complete surgical excision during the first time. Identifying the retroperitoneal space and ureter and correcting pelvic anatomy are the keys of success in treating DIE patients." Htut HT, Liu HM, Lee CL. Laparoscopic Excision of Severe Deep Infiltrating Endometriosis. Gynecol Minim Invasive Ther. 2022 Feb 14;11(1):76-77.
"The safe and complete excision of bladder endometriosis relies on the understanding of surgical anatomy, the multidisciplinary aspect of patient care, and the standardization of the surgical approach." Nguyen DB, Arendas K, Jago CA, Warren J, Singh SS. Stepwise approach to the laparoscopic excision of bladder endometriosis. Fertil Steril. 2022 Jan;117(1):225-227.
“Both types of treatment, surgical and pharmacological, effectively improved pain symptoms associated with DIE. However, improvement in chronic pelvic pain, dyschezia and deep dyspareunia was greater and longer-lasting after surgery.” Gabriela Pravatta Rezende, Marina Capovilla Venturini, Lucas Nobushy Kawagoe, Daniela Angerame Yela Gomes & Cristina Laguna Benetti-Pinto (2022) Surgery vs. hormone-based treatment for pain control in deep infiltrating endometriosis: a retrospective cohort study, Current Medical Research and Opinion.
"Narrow excision near the edge of the endometrioma and primary sphincteroplasty can be successfully used to manage these conditions. However, early diagnosis and treatment are important to preventing progressive involvement in the surrounding tissues, most notably the anal sphincter, to decrease the risk of postoperative fecal incontinence...Early intervention can significantly improve patient quality of life, and the diagnosis can only be confirmed by histopathological examination." Hakami R, AlMansour S, Aloraini HM, Alturki NI, Alswayyed M, AlHarbi RA, Alkhayal K. Isolated Perianal Endometrioma: A Case Report and Literature Review. Am J Case Rep. 2022 Jan 4;23:e934745.
"Several studies have recently concluded that surgical removal of DE nodules might actually have a favorable impact on IVF outcomes. This is in contradiction to European Society of Human Reproduction and Embryology statement which stated that there was no evidence supporting surgical management of DE prior to ART to improve pregnancy rate; several studies have suggested that the surgical removal of DE nodules might actually have a favorable impact on IVF outcomes." Khan S, Lee CL. Treating Deep Endometriosis in Infertile Patients before Assisted Reproductive Technology. Gynecol Minim Invasive Ther. 2021 Nov 5;10(4):197-202.
"Diagnosis of endometriosis is made by laparoscopy, following an experience guided clinical decision, based on history, symptoms, clinical exam and imaging. Biochemical markers are not useful. For deep endometriosis, imaging is important before surgery, notwithstanding rather poor predictive values when confidence limits, the prevalence of the disease and the absence of stratification of lesions by size, localization and depth of infiltration, are considered. Surgery of endometriosis is based on recognition and excision. Since the surrounding fibrosis belongs to the body with limited infiltration by endometriosis, a rim of fibrosis can be left without safety margins. For deep endometriosis, this results in a conservative excision eventually with discoid excision or short bowel resections. For cystic ovarian endometriosis superficial destruction, if complete, should be sufficient. Understanding pathophysiology is important for the discussion of early intervention during adolescence." Koninckx PR, Fernandes R, Ussia A, Schindler L, Wattiez A, Al-Suwaidi S, Amro B, Al-Maamari B, Hakim Z, Tahlak M. Pathogenesis Based Diagnosis and Treatment of Endometriosis. Front Endocrinol (Lausanne). 2021 Nov 25;12:745548.
"In general, the consensus among surgeons is that all visible lesions should be removed for prolonged improvement of symptoms. In addition, a specialized surgery should be taken into account to preserve organ functions, to reduce complications, and for nerve sparing." Angioni S, Nappi L, Sorrentino F, Peiretti M, Daniilidis A, Pontis A, Tinelli R, D'Alterio MN. Laparoscopic treatment of deep endometriosis with a diode laser: our experience. Arch Gynecol Obstet. 2021 Nov;304(5):1221-1231.
Endometriosis surgery provides significant improvement in DDyspareunia." Crispi CP Jr, Crispi CP, de Oliveira BRS, de Nadai Filho N, Peixoto-Filho FM, Fonseca MF. Six-month follow-up of minimally invasive nerve-sparing complete excision of endometriosis: What about dyspareunia? PLoS One. 2021 Apr 23;16(4):e0250046.
“Laparoscopic excision of endometriosis offers improvement in all quality-of-life domains as measured by the EHP-30, including a reduction in pain, an effect that may persist for up to 6.8 years. These findings suggest that laparoscopic excision of endometriosis with uterine preservation can be considered as an option for discussion during counseling for treatment of endometriosis.” Rindos NB, Fulcher IR, Donnellan NM. Pain and Quality of Life after Laparoscopic Excision of Endometriosis. J Minim Invasive Gynecol. 2020 Nov-Dec;27(7):1610-1617.e1.
"As shown in this case, the laparoscopic nerve-sparing complete excision of endometriosis is a feasible and reproducible technique in expert hands and, as reported in the literature, offers good results in terms of bladder morbidity reduction with higher satisfaction than the classical technique." Ceccaroni M, Clarizia R, Roviglione G. Nerve-sparing Surgery for Deep Infiltrating Endometriosis: Laparoscopic Eradication of Deep Infiltrating Endometriosis with Rectal and Parametrial Resection According to the Negrar Method. J Minim Invasive Gynecol. 2020 Feb;27(2):263-264.
"All suspected endometriosis lesions should be surgically excised for optimization of treatment and prevention of malignant transformation. If hormone replacement therapy is initiated, combined estrogen and progestin is recommended, even in the setting of previous hysterectomy, given the risk of disease reactivation and malignant transformation of endometriotic lesions." Ladanyi C, Boyd S, Sticco P, Mohling S. Postmenopausal endometriosis, where are we now? Curr Opin Obstet Gynecol. 2019 Aug;31(4):267-278.
“Deep infiltrating endometriosis is a complex disease associated with significant morbidity and requires highly trained, multidisciplinary team approach for safe and efficient excision." Graham A, Chen S, Skancke M, Moawad G, Obias V. A review of deep infiltrative colorectal endometriosis treated robotically at a single institution. Int J Med Robot. 2019 Aug;15(4):e2001.
“Laparoscopic surgical excision of bladder nodules has been demonstrated to be effective in relieving associated painful symptoms...Laparoscopic excision of anterior compartment endometriosis is [also] effective in restoring fertility in patients with otherwise-unexplained infertility and in treating endometriosis-related symptoms.” Centini G, Afors K, Alves J, Argay IM, Koninckx PR, Lazzeri L, Monti G, Zupi E, Wattiez A. Effect of Anterior Compartment Endometriosis Excision on Infertility. JSLS. 2018 Oct-Dec;22(4).
"Sacrospinous ligament excision relieved pain caused by endometriosis, so it may be applicable to the endometriosis patients with sacrospinous ligament infiltration or severe pain." Li J, Yao X, Zhang J. Treatment of pelvic cavity pain caused by endometriosis with excision of invaded sacrospinous ligament. Pak J Med Sci. 2018 Sep-Oct;34(5):1200- 1203.
"[Excisional] surgery is the treatment of choice because medical management alone commonly fails in controlling the symptoms although recurrence is very high after surgical treatment...Lack of complete surgical excision was another independent risk factor for recurrence of disease." Ianieri MM, Mautone D, Ceccaroni M. Recurrence in Deep Infiltrating Endometriosis: A Systematic Review of the Literature. J Minim Invasive Gynecol. 2018 Jul Aug;25(5):786-79.
"Surgical excision of endometriosis is an essential tool for the management of symptomatic disease...With appropriate technique, the rate of intraoperative complication, including bowel, bladder and ureteral injury as well as hematoma and bleeding, is approximately 1%. Postoperative complications, including drop in hemoglobin, urinary retention, cystitis, abdominal wall hematoma are usually minor and reoperation rates are well under 1%. Thorough dissection of the retroperitoneum facilitates complete excision of endometriosis with a minimum of morbidity." Gingold JA, Falcone T. The Retroperitoneal Approach to Endometriosis. J Minim Invasive Gynecol. 2017 Mar 3.
"Laparoscopically assisted ureterolyses, ureteral reanastomoses, and ureteral reimplantation are feasible, safe, and effective treatments for ureteral endometriosis. Complete laparoscopic excision is possible with minimal complications, which seem to be associated with the number of incisions. Ureteral endometriosis should be suspected in all cases of deep infiltrating endometriosis." Alves J, Puga M, Fernandes R, Pinton A, Miranda I, Kovoor E, Wattiez A. Laparoscopic Management of Ureteral Endometriosis and Hydronephrosis Associated with Endometriosis. J Minim Invasive Gynecol. 2017 Mar - Apr;24(3):466-472.
At “12 months postsurgery, symptoms of dysmenorrhea, dyschezia, and chronic pelvic pain secondary to endometriosis showed a significantly greater improvement with laparoscopic excision compared with ablation.” Pundir J, Omanwa K, Kovoor E, Pundir V, Lancaster G, Barton-Smith P. Laparoscopic Excision Versus Ablation for Endometriosis-associated Pain: An Updated Systematic Review and Meta-analysis. J Minim Invasive Gynecol. 2017 JulAug;24(5):747-756.
"Medical management of ovarian endometriomas is not recommended. Operative laparoscopy is the treatment of choice. Although considered a simple procedure, ovarian cystectomy requires a precise and correct technique in order to preserve ovarian function We aim for complete surgical excision in order to avoid leaving disease behind." López de la Torre MA, Abrao HM, Fernandes LF, Kho RM, Abrao MS. Ten Principles for Safe Surgical Treatment of Ovarian Endometriosis. J Minim Invasive Gynecol. 2017 Feb;24(2):203-204.
"…Surgical excision of endometriosis is a feasible and good treatment option for pain relief and improvement of quality of sex life in symptomatic women with endometriosis." Fritzer N, Hudelist G. Love is a pain? Quality of sex life after surgical resection of endometriosis: a review. Eur J Obstet Gynecol Reprod Biol. 2017 Feb;209:72-76.
“Knowledge of pelvic anatomy is crucial for surgeon preparation to completely excise the endometriosis, when feasible, and with the lowest complication rate.” Abrao, MS. Pillars for Surgical Treatment of Bowel Endometriosis. Journal of Minimally Invasive Gynecology, May–June, 2016, Volume 23, Issue 4, Pages 461–4620.
“Endometriotic lesion removal significantly alters the inflammatory profile both locally and systemically in women with endometriosis. Our findings indicate that ectopic lesions are the major drivers of systemic inflammation in endometriosis.” Monsanto SP, Edwards AK, Zhou J, Nagarkatti P, Nagarkatti M, Young SL, Lessey BA, Tayade C. Surgical removal of endometriotic lesions alters local and systemic proinflammatory cytokines in endometriosis patients. Fertil Steril. 2016 Apr;105(4):968-977.
“Radical laparoscopic excision of endometriosis offers an effective treatment option and offers a significant improvement in dyspareunia and quality of sex life.” Fritzer N, Tammaa A, Haas D, Oppelt P, Renner S, Hornung D, Wölfler M, Ulrich U, Hudelist G. When sex is not on fire: a prospective multicentre study evaluating the short-term effects of radical resection of endometriosis on quality of sex life and dyspareunia. Eur J Obstet Gynecol Reprod Biol. 2016 Feb;197:36-40.
"Patients had significantly improved pain symptoms and quality of life after excision surgery, whether or not DRPs were present. This study demonstrated that a DRP may be a manifestation of endometriosis (even with a clear surface of the pocket), so that DRPs should be excised to achieve optimal excision of endometriosis." Yeung PP Jr, Logan I, Gavard JA. Deep Retraction Pockets, Endometriosis, and Quality of Life. Front Public Health. 2016 May 9;4:85.
"GnRHa administration is followed by a temporary improvement of pain in patients with incomplete surgical treatment. It seems that it has no role on post-surgical pain when the surgeon is able to completely excise DIE implants." Angioni S, Pontis A, Dessole M, Surico D, De Cicco Nardone C, Melis I. Pain control and quality of life after laparoscopic en-block resection of deep infiltrating endometriosis (DIE) vs. incomplete surgical treatment with or without GnRHa administration after surgery. Arch Gynecol Obstet. 2015 Feb;291(2):363-70.
“Comparing with incomplete excision, the complete excision of DIE significantly decreased the post-operative pain and the recurrence rate. Although incomplete excision with post-operative GnRHa is efficient with respect to pain, the side effects of the drugs and the recurrence rate after cessation of the drugs must be considered. So complete excision of DIE is the first surgical treatment of choice.” Cao Q, Lu F, Feng WW, Ding JX, Hua KQ. Comparison of complete and incomplete excision of deep infiltrating endometriosis. Int J Clin Exp Med. 2015 Nov 15;8(11):21497- 506.
“This risk of reoperation for chronic pelvic pain following complete laparoscopic excision of endometriosis is low for patients managed in a multidisciplinary pelvic pain center. The majority of patients with chronic pelvic pain and endometriosis have additional related comorbidities. This preliminary data suggests that a thorough approach that addresses these additional processes that contribute to chronic pelvic pain may be a key factor in maintaining such reoperation rates lower than previously reported for patients with endometriosis.” Davison, J et al., Surgical Management of Endometriosis: Reoperation Rates Using Multimodal and Multidisciplinary Management Techniques, An Interim Analysis. Journal of Minimally Invasive Gynecology , November–December, 2015, Volume 22, Issue 6, Supplement, Page S54.
“Laparoscopic excision of endometriosis has been shown to significantly reduce pain and improve quality of life.” Nesbitt-Hawes, Erin M. et al., “The Surgical Treatment of Severe Endometriosis Positively Affects the Chance of Natural or Assisted Pregnancy Postoperatively.” BioMed Research International 2015 (2015): 438790.
“In [the preclinical model], we demonstrate that endometriosis pain is alleviated by surgical excision of the ectopic lesion or drainage of its cysts, providing support for the clinical observation that endometriosis pain is dependent upon the ongoing presence of the lesions.” Alvarez P, Giudice LC, Levine JD. Impact of surgical excision of lesions on pain in a rat model of endometriosis. Eur J Pain. 2015 Jan;19(1):103-10.
“Laparoscopic excision of endometriosis has been shown to significantly reduce pain and improve quality of life.” Nesbitt-Hawes, Erin M. et al., “The Surgical Treatment of Severe Endometriosis Positively Affects the Chance of Natural or Assisted Pregnancy Postoperatively.” BioMed Research International 2015 (2015): 438790.
“The surgical approach to treatment has a positive impact not only on organ impairment but also on sexual function in women affected by DIE.” Di Donato N, Montanari G, Benfenati A, Monti G, Leonardi D, Bertoldo V, Facchini C, Raimondo D, Villa G, Seracchioli R. Sexual function in women undergoing surgery for deep infiltrating endometriosis: a comparison with healthy women. J Fam Plann Reprod Health Care. 2015 Oct;41(4):278-83.
"A high recurrence rate of 62% is reported in advanced stages of endometriosis in which the ovaries were conserved. Ovarian conservation carries a 6 fold risk of recurrent pain and 8 folds risk of reoperation. The decision has to be weighed taking into consideration the patient's age and the impact of early menopause on her life style. The recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease. Surgical effort should always aim to eradicate the endometriotic lesions completely to keep the risk of recurrence as low as possible." Rizk B, Fischer AS, Lotfy HA, Turki R, Zahed HA, Malik R, Holliday CP, Glass A, Fishel H, Soliman MY, Herrera D. Recurrence of endometriosis after hysterectomy. Facts Views Vis Obgyn. 2014;6(4):219-27.
“Many great debates on the surgical management of endometriosis [exist]…there is general consensus that excision is best for optimal surgical outcome.” Falcone T, Wilson JR. Surgical management of endometriosis: excision or ablation. J Minim Invasive Gynecol. 2014 Nov-Dec;21(6):969.
“Hormonal suppression improves symptoms, but should not be used to diagnose endometriosis, and is not shown to be effective in preventing disease recurrence nor in improving fertility. The goal of surgical management should be optimal removal or treatment of disease and should include measures for adhesion prevention. Rates of recurrence of endometriosis depend on the surgical completeness of removing the disease.” Yeung P Jr . The laparoscopic management of endometriosis in patients with pelvic pain. Obstet Gynecol Clin North Am. 2014 Sep;41(3):371-83.
“Excision of lesions could be preferential with regard to the possibility of retrieving samples for histology. Furthermore, ablative techniques are unlikely to be suitable for advanced forms of endometriosis.” G.A.J. Dunselman, N. Vermeulen, C. Becker, C. Calhaz-Jorge, T. D'Hooghe, B. De Bie, O. Heikinheimo, A.W. Horne, L. Kiesel, A. Nap, A. Prentice, E. Saridogan, D. Soriano, W. Nelen. ESHRE guideline: Management of Women with Endometriosis. Hum. Reprod. (2014) 29 (3): 400-412.
“Surgical treatment of endometriosis provides symptom reduction for up to 5 years. In some limited areas such as deep dyspareunia, excision is more effective than ablation.” Healey M, Cheng C, Kaur H. To excise or ablate endometriosis? A prospective randomized double-blinded trial after 5-year follow-up. J Minim Invasive Gynecol. 2014 Nov-Dec;21(6):999-1004.
“Ablative techniques, on the other hand, are ‘unlikely to be suitable for advanced forms of endometriosis.’” [Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, D'Hooghe T, De Bie B, Heikinheimo O, Horne AW, Kiesel L, Nap A, Prentice A, Saridogan E, Soriano D, Nelen W. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014 Mar;29(3):400-12.
“The recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease. Surgical effort should always aim to eradicate the endometriotic lesions completely to keep the risk of recurrence as low as possible.” Rizk B, Fischer AS, Lotfy HA, et al., Recurrence of endometriosis after hysterectomy. Facts, Views & Vision in ObGyn. 2014;6(4):219-227.
“A well-trained interdisciplinary team can perform treatment of deep infiltrating endometriosis laparoscopically with low incidence of major complications as anastomotic leakage or rectovaginal fistula. Criteria of complete endometriosis restoration of the rectum can be achieved by total or subtotal rectal excision.” Bachmann R, Bachmann C, Lange J, Krämer B, Brucker SY, Wallwiener D, Königsrainer A, Zdichavsky M. Surgical outcome of deep infiltrating colorectal endometriosis in a multidisciplinary setting. Arch Gynecol Obstet. 2014 Nov;290(5):919-24.
“There is good evidence that in experienced hands laparoscopic [resection] surgery helps in long-term symptomatic relief, improves pregnancy rates and reduces recurrence of disease with largely avoiding complications.” Shah PR, Adlakha A. Laparoscopic management of moderate: Severe endometriosis. J Minim Access Surg. 2014 Jan;10(1):27- 33.
“Multidisciplinary laparoscopic treatment has become the standard of care and depending on size of the lesion and site of involvement full-thickness disc excision or bowel resection is performed by an experienced colorectal surgeon. Anastomotic complications occur around 1%. Wolthuis AM, Tomassetti C. Long-term outcome after bowel resection for severe endometriosis is good with a pregnancy rate of 50%.” Multidisciplinary laparoscopic treatment for bowel endometriosis. Best Pract Res Clin Gastroenterol. 2014 Feb;28(1):53-67.
“There is good evidence that in experienced hands laparoscopic [resection] surgery helps in long-term symptomatic relief, improves pregnancy rates and reduces recurrence of disease with largely avoiding complications.” Shah PR, Adlakha A. Laparoscopic management of moderate: Severe endometriosis. J Minim Access Surg. 2014 Jan;10(1):27- 33.
“If the treating surgeon is not familiar with all appearances, endometriosis may be missed and left untreated in his or her patients; you see only what you recognize. This is particularly relevant in deep infiltrating disease, where sometimes endometriosis is hidden beneath the surface.” Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, D'Hooghe T, De Bie B, Heikinheimo O, Horne AW, Kiesel L, Nap A, Prentice A, Saridogan E, Soriano D, Nelen W. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014 Mar;29(3):400-12.
"Surgical excision of deep infiltrating endometriosis is feasible and improves dyspareunia and quality of sex life significantly." Fritzer N, Tammaa A, Salzer H, Hudelist G. Dyspareunia and quality of sex life after surgical excision of endometriosis: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2014 Feb;173:1-6.
“Th[is] study demonstrated no clear association between the depth of excision of endometriosis with urinary and bowel dysfunction. The differences in urinary stress incontinence and bowel dysfunction may be explained by DIE itself causing damage to the hypogastric plexus.” Li YH, De Vries B, Cooper M, Krishnan S. Bowel and bladder function after resection of deeply infiltrating endometriosis. Aust NZJ Obstet Gynaecol. 2014 Jun;54(3):218-2.
'Complete resection of all visible foci of disease offers the best control of symptoms.’ (Rimbach S, Ulrich U, Schweppe KW. Surgical Therapy of Endometriosis: Challenges and Controversies. Geburtshilfe Frauenheilkd. 2013 Sep;73(9):918-923).
“The issue of appropriate Laparoscopic surgical training is considered vital and there are strong arguments for standardization of what constitutes the relevant experience and expertise for those undertaking complex Laparoscopic surgery for endometriosis. Crucial aspects in planning Laparoscopic surgery are that surgery should be carried out in the most appropriate setting which can ensure adequate preoperative counseling, appropriate surgical expertise (to ensure the most appropriate procedure is undertaken by the most experienced surgeon at the most appropriate time), adequate technical resources and post-operative support care…It is also important, particularly in cases of more severe endometriosis, that surgeons consider the option of limiting surgical excision at an initial operation in order to refer to a surgeon better equipped to deal with endometriosis, as the first definitive surgical intervention has been shown to deliver the greatest benefit…there is unanimous consensus over the recommendation to excise lesions where possible, especially deep endometrioctic lesions, which is felt by most surgeons to give a more thorough removal of disease.” Johnson NP, Hummelshoj L; World Endometriosis Society Montpellier Consortium. Consensus on Current Management of Endometriosis. Hum Reprod. 2013 Jun;28(6):1552-68.
"After surgical treatment [excision] of endometriosis, the pregnancy and live birth rates seem to be improved. Reproductive outcome is closely associated with the AFS score. Bilaterality of endometriosis does not affect pregnancy outcome." Cirpan T, Akman L, Yucebilgin MS, Terek MC, Kazandi M. Reproductive outcome after surgical treatment of endometriosis--retrospective analytical study. Ginekol Pol. 2013 Dec;84(12):1041-4.
“The success of treatment depends on the resorption of all residual visible lesions and the eradication of microscopic implants.” Ilker Selcuk, Gurkan Bozdag. Recurrence of endometriosis; risk factors, mechanisms and biomarkers; review of the literature. J Turk Ger Gynecol Assoc. 2013; 14(2): 98–103 (Print).
“After the evaluation of 121 patients following conservative laparoscopic surgery, Ghezzi et al., reported that the left sided endometriomas recur more frequently, whereas Jones and Sutton found that bilateral cysts were more likely to recur than single cysts after the evaluation of 73 patients following consecutive laparoscopic ablation. Saleh and Tulandi evaluated 231 patients after the laparoscopic excision of endometrioma cysts and found that the reoperation rate was higher in women with larger cysts; Koga et al., also reported similar findings after following-up 224 patients post-operatively for a minimum of 2 years. Busacca et al., followed-up 366 patients after laparoscopic endometrioma excision and reported that the advanced stage disease and previous surgery for endometriosis were two risk factors for recurrence and that the rate of recurrence increased with an extended follow-up period; they also found that the cyst recurrence was mostly associated with the pain recurrence. Porpora et al., followed-up 166 patients after laparoscopic endometrioma cystectomy and found that prior surgery, pelvic adhesions and high rAFS score were all negative prognostic factors for recurrence. Fedele et al., evaluated 47 symptomatic bladder endometriosis patients and found that the radicality of surgery was important for recurrence. Vignali et al.,reported that the completeness of the first surgery was a prognostic factor for recurrence after a 12 month follow-up period in 115 symptomatic patients who were operated upon for deep infiltrating endometriosis. Parazzini et al., reported that the advanced stage disease at initial surgery had a higher recurrence rate and Busacca et al., showed deep endometriosis, younger age, stage 3 or 4 disease and time passed after surgery were all risk factors for recurrence.” Selçuk İ, Bozdağ G. Recurrence of endometriosis; risk factors, mechanisms and biomarkers; review of the literature. Journal of the Turkish German Gynecological Association. 2013;14(2):98-103.
“Excision of endometriosis showed a significant reduction in all pain scores except bowel symptoms, as well as significant improvement in quality of life." Yeung P Jr, Tu F, Bajzak K, Lamvu G, Guzovsky O, Agnelli R, Peavey M, Winer W, Albee R, Sinervo K. A pilot feasibility multicenter study of patients after excision of endometriosis. JSLS. 2013 Jan-Mar;17(1):88-94.
"In cases of endometriosis, complete excision of endometriosis and ovarian tissue at the time of initial surgery prevents recurrence of endometriosis, subsequent development of ORS and possible ovarian malignant transformation." Kho RM, Abrao MS. Ovarian remnant syndrome: etiology, diagnosis, treatment and impact of endometriosis. Curr Opin Obstet Gynecol. 2012 Aug;24(4):210-4.
"Complete excision of endometriosis, including vaginal resection, seems to offer a significant improvement in sexual functioning, quality of life and pelvic pain in symptomatic patients with deeply infiltrating endometriotic nodules in the posterior fornix of the vagina. This surgery may be associated with complications and adverse new-onset symptoms, and should be performed only after thorough consultation with the patient." Setälä M, Härkki P, Matomäki J, Mäkinen J, Kössi J. Sexual functioning, quality of life and pelvic pain 12 months after endometriosis surgery including vaginal resection. Acta Obstet Gynecol Scand. 2012 Jun;91(6):692-8.
“…laparoscopic resection of the mid/low rectum for endometriosis can be performed safely with acceptable rates of morbidity/reoperation and with low rates of specific complications, including anastomotic leak and rectovaginal fistula. The very high surgical volume of the operating surgeon is probably one of the most important factors in order to maximize postoperative outcomes.” Ruffo G, Sartori A, Crippa S, Partelli S, Barugola G, Manzoni A, Steinasserer M, Minelli L, Falconi M. Laparoscopic rectal resection for severe endometriosis of the mid and low rectum: technique and operative results. Surg Endosc. 2012 Apr;26(4):1035-40.
“CO2 laser laparoscopic radical excision of DIE with colorectal extension and laparoscopic segmental bowel resection in centers of expertise is associated with good clinical outcome.“ Meuleman C, Tomassetti C, D’Hooghe TM. Clinical outcome after laparoscopic radical excision of endometriosis and laparoscopic segmental bowel resection. Curr Opin Obstet Gynecol. 2012 Aug;24(4):245-52.
“Laparoscopic treatment of ureteric endometriosis is feasible. Intrinsic ureteric endometriosis is quite frequent in severe ureterohydronephrosis. Complete excision of the disease is essential to improve pain symptomatology and to prevent recurrence of disease. Long term follow up is required to exclude any stenosis.” Miranda-Mendoza I, Kovoor E, Nassif J, Ferreira H, Wattiez A. Laparoscopic surgery for severe ureteric endometriosis. Eur J Obstet Gynecol Reprod Biol. 2012 Jul 22.
"Sexual desire, satisfaction with sex and pelvic problem interference with intercourse are significantly improved after 6 months from laparoscopic excision of DIE combined with postoperative COC therapy. No difference in sexual outcomes was detected between patients submitted to intestinal resection and nodule excision." Mabrouk M, Montanari G, Di Donato N, Del Forno S, Frascà C, Geraci E, Ferrini G, Vicenzi C, Raimondo D, Villa G, Zukerman Z, Alvisi S, Seracchioli R. What is the impact on sexual function of laparoscopic treatment and subsequent combined oral contraceptive therapy in women with deep infiltrating endometriosis? J Sex Med. 2012 Mar;9(3):770-8.
“One year after laser ablation for painful pelvic endometriosis, 29% of women who continued to be symptomatic were found to have progressive disease and 42% static disease at second look laparoscopy. Many women may undergo additional surgical intervention as a result of persistent or worsening of symptoms. The reoperation rate after laparoscopic treatment of endometriosis has been found to be 21% at 2 years and 58% at 7 years. Endometriosis was most likely to recur close to the original area of involvement, which may be the result of incomplete excision or ablation.” Giudice, Linda, Johannes Evers, DL Healy. Endometriosis: Science and Practice. Chichester, West Sussex: Wiley-Blackwell, 2012 (Print).
“Medical therapy does not provide for adequate pain relief, and an effective management option to reduce pelvic pain appears to be complete laparoscopic removal of as many endometriotic lesions as possible…The addition of radical removal of deep endometriotic lesions to conservative laparoscopic surgery markedly reduces the severity of dysmenorrhea and the rate of recurrent pelvic pain. Although the surgical procedure is technically demanding, the levels of peri-operative complications and morbidity are acceptable.” Hidaka T, Nakashima A, Hashimoto Y, Saito S. Effects of laparoscopic radical surgery for deep endometriosis on endometriosis-related pelvic pain. Minim Invasive Ther Allied Technol. 2012 Sep;21(5):355-61.
“The current evidence strongly supports the effectiveness of radical laparoscopic resection in relieving endometriosis- associated symptoms and enhancing psychological well-being. In addition, studies suggest a general improvement of quality of life.” Fritzer N, Tammaa A, Salzer H, Hudelist G. Effects of surgical excision of endometriosis regarding quality of life and psychological well-being: a review. Womens Health (Lond Engl). 2012 Jul;8(4):427-35.
“CO2 laser laparoscopic radical excision of DIE with colorectal extension and laparoscopic segmental bowel resection in centers of expertise is associated with good clinical outcome.“ Meuleman C, Tomassetti C, D’Hooghe TM. Clinical outcome after laparoscopic radical excision of endometriosis and laparoscopic segmental bowel resection. Curr Opin Obstet Gynecol. 2012 Aug;24(4):245-52.
“Laparoscopic treatment of ureteric endometriosis is feasible. Intrinsic ureteric endometriosis is quite frequent in severe ureterohydronephrosis. Complete excision of the disease is essential to improve pain symptomatology and to prevent recurrence of disease. Long term follow up is required to exclude any stenosis.” Miranda-Mendoza I, Kovoor E, Nassif J, Ferreira H, Wattiez A. Laparoscopic surgery for severe ureteric endometriosis. Eur J Obstet Gynecol Reprod Biol. 2012 Jul .
“Complete excision of endometriosis, including vaginal resection, seems to offer a significant improvement in sexual functioning, quality of life and pelvic pain in symptomatic patients with deeply infiltrating endometriotic nodules in the posterior fornix of the vagina.” Setälä M, Härkki P, Matomäki J, Mäkinen J, Kössi J. Sexual functioning, quality of life and pelvic pain 12 months after endometriosis surgery including vaginal resection. Acta Obstet Gynecol Scand. 2012 Jun;91(6):692-8.
“Thus, LAPEX remains the most minimally invasive, highly cost-effective option, particularly when early diagnosis is conferred.” Mabrouk M, Montanari G, Guerrini M, Villa G, Solfrini S, Vicenzi C, et. al. Does laparoscopic management of deep infiltrating endometriosis improve quality of life? A prospective study. Health Qual Life Outcomes. 2011 Nov 6;9:98.
“…laparoscopic excision can “significantly reduce pain and improve quality of life in women with endometriosis…in deep-infiltrating rectovaginal endometriosis, for example, radical excision including bowel surgery has been reported to alleviate symptoms in up to 80% of affected women... recurrence seems to originate from residual lesions, which have been left behind in the course of the initial surgery.” Gong Y, Tempfer CB. Regional lymphatic spread in women with pelvic endometriosis. Med Hypotheses. 2011 Apr;76(4):560-3.
“…surgeons trained in laparoscopic surgery but without specific expertise in endometriosis surgery may be less proficient in surgery for endometriomas. Specimens obtained via surgery performed by residents have statistically significantly more ovarian tissue when compared with those obtained by experienced surgeons with years of practice in the field of reproductive and endometriosis surgery. In experienced hands, laparoscopic stripping of endometriomas appears to be a technique that does not significantly damage the ovarian tissue.” Muzii L, Marana R, Angioli R, Bianchi A, Cucinella G, Vignali M, Benedetti Panici P, Busacca M. Histologic analysis of specimens from laparoscopic endometrioma excision performed by different surgeons: does the surgeon matter? Fertil Steril. 2011 May;95(6):2116-9.
“Pain, sexual function and QOL improved significantly and were associated with a good fertility rate and a low complication and recurrence rate after a CO2 laser laparoscopic radical excision of endometriosis with colorectal wall invasion combined with laparoscopic segmental bowel resection and reanastomosis.” Meuleman C, Tomassetti C, D’Hoore A, Buyens A, Van Cleynenbreugel B, Fieuws S, Penninckx F, Vergote I, D’Hooghe T. Clinical outcome after CO2 laser laparoscopic radical excision of endometriosis with colorectal wall invasion combined with laparoscopic segmental bowel resection and reanastomosis. Hum Reprod. 2011 Sep;26(9):2336-43.
“Laparoscopic excision of DIE lesions significantly improves general health and psycho-emotional status at six months from surgery without differences between patients submitted to intestinal segmental resection or intestinal nodule shaving.” Mabrouk M, Montanari G, Guerrini M, Villa G, Solfrini S, Vicenzi C, Mignemi G, Zannoni L, Frasca C, Di Donato N, Facchini C, Del Forno S, Geraci E, Ferrini G, Raimondo D, Alvisi S, Seracchioli R. Does laparoscopic management of deep infiltrating endometriosis improve quality of life? A prospective study. Health Qual Life Outcomes. 2011 Nov 6;9:98.
“We believe that, besides endometriosis in itself, the overall quality of surgery may have a major role in determining damage to the ovary. In recent years, surgeons dedicated to the treatment of endometriosis have refined the technique of laparoscopic surgery for the excision of endometriomas, with particular attention in developing the correct plane of cleavage and in the judicious use of electrosurgery...Quality of the surgery, and not surgery per se, may be important. Surgery is the gold standard treatment for ovarian endometriomas, but it should be performed with proper techniques by specifically trained surgeons. It's the singer, not the song.” Muzii L, Miller CE. The singer, not the song. J Minim Invasive Gynecol. 2011 Sep-Oct;18(5):666-7.
"Complete laparoscopic excision of endometriosis in teenagers--including areas of typical and atypical endometriosis--has the potential to eradicate disease. These results do not depend on postoperative hormonal suppression." Yeung P Jr, Sinervo K, Winer W, Albee RB Jr. Complete laparoscopic excision of endometriosis in teenagers: is postoperative hormonal suppression necessary? Fertil Steril. 2011 May;95(6):1909-12, 1912.e1.
“The literature supports fertility-sparing laparoscopic excision of deeply infiltrating endometriosis as a safe and effective procedure with a low short-term complication rate.” Pandis GK, Saridogan E, Windsor AC, Gulumser C, Cohen CR, Cutner AS. Short-term outcome of fertility-sparing laparoscopic excision of deeply infiltrating pelvic endometriosis performed in a tertiary referral center. Fertil Steril. 2010 Jan;93(1):39-45.
"All the stages of disease are present in the adolescent, including stages III and IV. The laparoscopic excision of endometriosis has a positive effect on the relief of pain symptoms and on the improvement in quality of life in the adolescent." Roman JD. Adolescent endometriosis in the Waikato region of New Zealand--a comparative cohort study with a mean follow-up time of 2.6 years. Aust N Z J Obstet Gynaecol. 2010 Apr;50(2):179-83.
"Laparoscopic excision of endometriosis significantly reduces pain and improves quality of life as measured by both the EQ-5D index and the EQ-5D VAS, with a low complication rate." Roman JD. Surgical treatment of endometriosis in private practice: cohort study with mean follow-up of 3 years. J Minim Invasive Gynecol. 2010 Jan-Feb;17(1):42-6.
“Laparoscopy is highly cost effective in initial management of young women with infertility, particularly when infertility treatment dropout rates exceed 9% per cycle.” Moayeri SE, Lee HC, Lathi RB, Westphal LM, Milki AA, Garber AM. Laparoscopy in women with unexplained infertility: a costeffectiveness analysis. Fertil Steril. 2009 Aug;92(2):471-80.
“…the learning curve for difficult surgical procedures such as the adequate treatment of rectovaginal endometriosis is the most plausible explanation for higher recurrence rates in the early patients because of the surgeon’s limited technical skills. Therefore, this unintentionally produced a subgroup of women in whom part of the disease is often left behind untouched. The notion of complete and incomplete surgery depends on the surgeon’s impression and even in supposedly complete surgery, there might be something that remains behind that cannot be seen during the operation. Surgical completeness is a major continuing problem in the conservative treatment of endometriosis, mainly in women with deeply invasive disease because the deeper the lesion, the more difficult the dissection from the surrounding tissue and therefore, complete excision…the aim of treatment should be to remove all of the extrauterine disease while retaining all the healthy tissue, including the uterus and ovaries. If all endometriotic tissue can be removed, excellent long-term results without the need for hysterectomy or oophorectomy can be obtained. There is also clear evidence that failure to remove all of the endometriotic tissue may result in persistent symptoms, even when the uterus and ovaries have been removed, and that these symptoms are cured by excising residual endometriotic tissue. Thus, the current investigation and previous studies indicate that both the recurrence of disease and reoperation are significantly more frequent in women who had an incomplete operation in the surgeon’s opinion. Considering that conservative treatment of rectovaginal endometriosis implies difficult and challenging surgery with potential complications, and the ability to perform a complete operation may have significant influence on the risk of disease recurrence. Management of deep endometriosis should be carried out in centers adequately staffed and equipped to ensure that appropriate treatment is available to most women who might benefit from this surgical approach.” Carmona F, Martínez-Zamora A, González X, Ginés A, Buñesch L, Balasch J. Does the learning curve of conservative laparoscopic surgery in women with rectovaginal endometriosis impair the recurrence rate? Fertil Steril. 2009 Sep;92(3):868-75.
"Extensive laparoscopic excision of DIE significantly improved IVF pregnancy rates of women with infertility-associated DIE." Bianchi PH, Pereira RM, Zanatta A, Alegretti JR, Motta EL, Serafini PC. Extensive excision of deep infiltrative endometriosis before in vitro fertilization significantly improves pregnancy rates. J Minim Invasive Gynecol. 2009 Mar-Apr;16(2):174-80.
"Diagnosis of the rectovaginal endometriosis is based on symptoms, vaginal and rectal examination, and auxiliary examination. Complete excision of endometriosis nodules is the main therapeutic method." Wang WX, Peng ZL. [Diagnosis and management of 57 cases with rectovaginal endometriosis]. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2009 Sep;38(5):531-4.
"These data suggest that when the surgical objective is complete eradication of endometriosis, the surgeon must be prepared to excise all lesions suggestive of endometriosis and tissue atypical in appearance as in most anatomic sites approximately 25% of atypical specimens proved to be endometriosis." Albee RB Jr, Sinervo K, Fisher DT. Laparoscopic excision of lesions suggestive of endometriosis or otherwise atypical in appearance: relationship between visual findings and final histologic diagnosis. J Minim Invasive Gynecol. 2008 Jan-Feb;15(1):32-7.
“Excision improves dyspareunia and quality of sex life.” Ferrero, Abbamonte, Giordano, Ragni, Remorgida. Deep dyspareunia & sex life after laparoscopic excision of endometriosis. HumReprod. 2007 22: 1142-1148.
“Laparoscopic laser excision of rectovaginal endometriosis is a safe procedure with similar, if not lower, complication rates to other published surgical series.” Slack A, Child T, Lindsey I, Kennedy S, Cunningham C, Mortensen N, Koninckx P, McVeigh E. Urological and colorectal complications following surgery for rectovaginal endometriosis. BJOG 2007;114:1278–1282.
“The recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease. Surgical effort should always aim to eradicate the endometriotic lesions completely to keep the risk of recurrence as low as possible.” Rizk B, Fischer AS, Lotfy HA, et al., Recurrence of endometriosis after hysterectomy. Facts, Views & Vision in ObGyn. 2014;6(4):219-227.
“Deep pelvic endometriosis surgery may need substantial excisions, which in turn expose to risks of injury to the pelvic nerves…key anatomical pitfalls must be known in order to limit the functional complications of the endometriotic surgical excision.” Fermaut M, Nyangoh Timoh K, Lebacle C, Moszkowicz D, Benoit G, Bessede T. Deep infiltrating endometriosis surgical management and pelvic nerves injury Gynecol Obstet Fertil. 2016 Apr 21.
“A well-trained interdisciplinary team can perform treatment of deep infiltrating endometriosis laparoscopically with low incidence of major complications as anastomotic leakage or rectovaginal fistula. Criteria of complete endometriosis restoration of the rectum can be achieved by total or subtotal rectal excision.” Bachmann R, Bachmann C, Lange J, Krämer B, Brucker SY, Wallwiener D, Königsrainer A, Zdichavsky M. Surgical outcome of deep infiltrating colorectal endometriosis in a multidisciplinary setting. Arch Gynecol Obstet. 2014 Nov;290(5):919-2.
“Th[is] study demonstrated no clear association between the depth of excision of endometriosis with urinary and bowel dysfunction. The differences in urinary stress incontinence and bowel dysfunction may be explained by DIE itself causing damage to the hypogastric plexus.” Li YH, De Vries B, Cooper M, Krishnan S. Bowel and bladder function after resection of deeply infiltrating endometriosis. Aust NZJ Obstet Gynaecol. 2014 Jun;54(3):218-24.
"Laparoscopic nerve-sparing complete excision of endometriosis seems to be feasible and offers good results in terms of bladder morbidity reduction with apparently higher satisfaction than classical technique." Landi S, Ceccaroni M, Perutelli A, Allodi C, Barbieri F, Fiaccavento A, Ruffo G, McVeigh E, Zanolla L, Minelli L. Laparoscopic nerve-sparing complete excision of deep endometriosis: is it feasible? Hum Reprod. 2006 Mar;21(3):774-81.
"Fertility-sparing laparoscopic excision of endometriosis with bowel resection results in improvements in all aspects of pain and quality of life. Results appear to parallel published data for conservative resection of endometriosis not involving bowel. For women with severe endometriosis involving bowel, this surgical treatment provides a viable alternative to pelvic clearance and successfully maintains fertility." Lyons SD, Chew SS, Thomson AJ, Lenart M, Camaris C, Vancaillie TG, Abbott JA. Clinical and quality-of-life outcomes after fertility-sparing laparoscopic surgery with bowel resection for severe endometriosis. J Minim Invasive Gynecol. 2006 Sep-Oct;13(5):436-41.
"Laparoscopic excision is currently the 'gold standard' approach for the management of endometriosis, and results may be improved with careful use of appropriate techniques and suitable adjuvant therapies." Garry R. The effectiveness of laparoscopic excision of endometriosis. Curr Opin Obstet Gynecol. 2004 Aug;16(4):299-303.
"Laparoscopic excision of endometriosis is more effective than placebo at reducing pain and improving quality of life. Surgery is associated with a 30% placebo response rate that is not dependent on severity of disease. Approximately 20% of women do not report an improvement after surgery for endometriosis." Abbott J, Hawe J, Hunter D, Holmes M, Finn P, Garry R. Laparoscopic excision of endometriosis: a randomized, placebo-controlled trial. Fertil Steril. 2004 Oct;82(4):878-84.
“Endometriosis is best treated by surgical excision. This can be accomplished either by excision of the endometriosis with reproductive tract preservation or by excision of endometriosis with hysterectomy. This latter approach eliminates endometriosis in the muscle of the uterus (where it is called adenomyosis) and is especially effective for pelvic pain." Reich H, Redan JA, Orbuch IK. Laparoscopic hysterectomy for advanced endometriosis including rectosigmoid disease. Surg Technol Int. 2004;13:121-36.
“Laparoscopic excision of endometriosis significantly reduces pain and improves quality of life for up to 5 years…[R]eturn of pain following laparoscopic excision is not always associated with clinical evidence of recurrence.” Abbott JA, Hawe J, Clayton RD, Garry R. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2–5 year follow. Hum. Reprod. (2003) 18 (9): 1922-1927.
“Aggressive laparoscopic excision of endometriosis carried out in a specialist center offers good symptom relief, especially for those with severe or debilitating symptoms. To ensure complete removal of all disease, intestinal surgery is required in most patients with complete obliteration of the cul-desac.” Redwine DB, Wright JT. Laparoscopic treatment of complete obliteration of the cul-de-sac associated with endometriosis: long-term follow-up of en bloc resection. Fertil Steril. 2001 Aug;76(2):358-65.
‘In a 24-month follow-up of 240 patients comparing excision alone, laser coagulation alone, or laser coagulation plus medical therapy at 1 year out, results found that 96% of excision patients were pain-free; 69% of coagulation were pain-free. Only 23% of coagulation patients were pain-free at 2 years out.’ Winkel CA, Bray M. Treatment of women with endometriosis using excision alone, ablation alone, or ablation in combination with leuprolide acetate. Proceedings of the Fourth World Congress on Endometriosis, Yokahama, Japan, 1996:55.
“Laparoscopic excision of endometriosis results in a low rate of minimal persistent/recurrent disease. The natural history of endometriosis after surgery suggests a rather static nature of the disease.” Redwine DB. Conservative laparoscopic excision of endometriosis by sharp dissection: life table analysis of reoperation and persistent or recurrent disease. Fertil Steril. 1991 Oct;56(4):628-34.